Dosing & Uses
Dosage Forms & Strengths
injectable solution (as tartrate)
- 1mg/mL
tablet (as tartrate)
- 25mg (generic)
- 50mg (generic, Lopressor)
- 100mg (generic, Lopressor)
tablet, extended-release (Toprol XL [as succinate])
- 25mg
- 50mg
- 100mg
- 200mg
capsule, extended-release (Kapspargo Sprinkle [as succinate])
- 25mg
- 50mg
- 100mg
- 200mg
Hypertension
Lopressor
- 100 mg/day PO initially in single dose or divided q12hr; may be increased at intervals of 1 week or longer; not to exceed 450 mg/day
Toprol XL
- 25-100 mg PO qDay initially; may be increased at intervals of 1 week or longer; usual range, 50-100 mg/day; not to exceed 400 mg/day
Kapspargo Sprinkles
- Initial dose: 25-100 mg PO qDay in a single dose; adjust dosage at weekly (or longer) intervals until optimum blood pressure reduction is achieved
- Dosages above 400 mg/day not studied
Acute Myocardial Infarction
Early treatment
Lopressor
- 5 mg rapid IV q2min, up to 3 doses; then, 15 minutes after last IV, 50 mg PO q6hr for 48 hours; then 50-100 mg PO q12hr
- If full IV dose not tolerated: 25-50 mg PO q6hr after last IV
Congestive Heart Failure
Toprol XL
- 25 mg PO qDay initially; increased every 2 weeks PRN; target dosage, 200 mg/day
- New York Heart Association (NYHA) class ≥II: Reduce dosage 12.5 mg/day
Kapspargo Sprinkle
- Prior to initiation, stabilize dose of other heart failure drug therapy and ensure patient is not fluid overloaded
- Initial dose: 25 mg PO qDay for 2 weeks
- Not suitable for initial therapy in patients who are expected to require a starting dose less than 25 mg/day
- Individualize dose and closely monitor during up-titration; double dose q2Weeks to the highest dosage level tolerated or up to 200 mg
Angina
Lopressor
- 100 mg/day PO initially divided q12hr; may be increased at intervals of 1 week or longer; not to exceed 400 mg/day
Toprol XL
- 100 mg/day PO initially; may be increased at intervals of 1 week or longer; not to exceed 400 mg/day
Kapspargo Sprinkle
- Usual initial dose: 100 mg PO qDay, given in a single dose; gradually increase dose at weekly intervals until optimum clinical response is achieved or there is a pronounced slowing of the heart rate
- Dosages above 400 mg/day have not been studied
- If treatment is to be discontinued, gradually reduce dose over a period of 1-2 weeks
Acute Tachyarrhythmia (Off-label)
5 mg IV over 1-2 minutes q5min; total dose not to exceed 15 mg
Migraine (Off-label)
Prophylaxis
Metoprolol tartrate: 50-100 mg PO q12hr
Atrial Fibrillation/Flutter or Supraventricular Tachycardia (Off-label)
2.5-5 mg IV q2-5min; not to exceed 15 mg over 10-15 minutes; maintenance: 25-100 mg PO q12hr
Dosing Modifications
Lopressor
- Renal impairment: No dosage adjustment necessary; systemic availability and half-life in patients with renal failure do not differ to a clinically significant degree from those in normal subjects
- Hepatic impairment: Since drug is primarily eliminated by hepatic metabolism, hepatic impairment may impact the pharmacokinetics of metoprolol; elimination half-life of metoprolol is considerably prolonged, depending on severity (up to 7.2 hr)
Kapspargo Sprinkle
- If a patient experiences symptomatic bradycardia, reduce dose
- If transient worsening of heart failure occurs, consider treating with increased doses of diuretics, lower dose or temporarily discontinuing treatment
- Do not increase until symptoms of worsening heart failure have been stabilized
- Initial difficulty with titration should not preclude later attempts to introduce Kapspargo Sprinkle
- or patients who are taking metoprolol succinate ER tablets at a dose of 25-200 mg PO qDay, substitute ER capsules for ER tablets, using the same total daily dose of metoprolol succinate
Dosing Considerations
Switching from immediate-release to extended-release: Use same total daily dose of metoprolol
Switching between oral and IV dosage forms: Equivalent beta-blocking effect is achieved in 2.5:1 (oral-to-IV) ratio
Dosage Forms & Strengths
injectable solution (as tartrate)
- 1mg/mL
tablet (as tartrate)
- 25mg (generic)
- 50mg (generic, Lopressor)
- 100mg (generic, Lopressor)
tablet, extended-release (Toprol XL [as succinate])
- 25mg
- 50mg
- 100mg
- 200mg
capsule, extended-release (Kapspargo Sprinkle [as succinate])
- 25mg
- 50mg
- 100mg
- 200mg
Hypertension
Lopressor
Toprol XL
- ≥6 years: 1 mg/kg PO qDay; not to exceed 50 mg/day initially; adjusted on basis of patient response; not to exceed 2 mg/kg/day or ≤200 mg/day
Kapspargo Sprinkle
- <6 years: Safety and efficacy not established
- ≥6 years: 1 mg/kg PO qDay, do not exceed 50 mg PO qDay; adjust dosage according to blood pressure response
- Doses >2 mg/kg (or >200 mg) qDay not studied
Use lower dosage in management of hypertension
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (0)
Serious - Use Alternative (34)
- acebutolol
acebutolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- artemether/lumefantrine
artemether/lumefantrine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- atenolol
atenolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- betaxolol
betaxolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- bisoprolol
bisoprolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- carvedilol
carvedilol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- celiprolol
celiprolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- chlorpromazine
metoprolol, chlorpromazine. Either increases levels of the other by decreasing metabolism. Contraindicated. Not all beta blockers share this interaction (e.g., atenolol, nadolol, sotalol do not interact).
- clonidine
clonidine, metoprolol. Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
- dacomitinib
dacomitinib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Avoid use with CYP2D6 substrates where minimal increases in concentration of the CYP2D6 substrate may lead to serious or life-threatening toxicities.
- digoxin
digoxin increases toxicity of metoprolol by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
- diltiazem
diltiazem, metoprolol. Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
- elvitegravir/cobicistat/emtricitabine/tenofovir DF
elvitegravir/cobicistat/emtricitabine/tenofovir DF increases levels of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Cobicistat is a CYP2D6 inhibitor; caution with CYP2D6 substrates for which elevated plasma concentrations are associated with serious and/or life-threatening events.
- esmolol
esmolol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- fexinidazole
fexinidazole, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Avoid coadministration of fexinidazole with drugs known to induce bradycardia. .
- fluoxetine
fluoxetine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- givosiran
givosiran will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of sensitive CYP2D6 substrates with givosiran. If unavoidable, decrease the CYP2D6 substrate dosage in accordance with approved product labeling.
- labetalol
labetalol and metoprolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- lofexidine
lofexidine, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Avoid coadministration with other drugs that decrease pulse or blood pressure to mitigate risk of excessive bradycardia and hypotension.
- lumefantrine
lumefantrine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- mavacamten
metoprolol, mavacamten. Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Expect additive negative inotropic effects of mavacamten and other drugs that reduce cardiac contractility.
- nadolol
metoprolol and nadolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- nebivolol
metoprolol and nebivolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- paroxetine
paroxetine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- penbutolol
metoprolol and penbutolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- pindolol
metoprolol and pindolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- propranolol
metoprolol and propranolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- quinidine
quinidine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. If concurrent therapy required, monitor cardiac function carefully (blood pressure, heart rate). A dosage adjustment may be required for both drugs.
- rivastigmine
metoprolol increases toxicity of rivastigmine by pharmacodynamic synergism. Avoid or Use Alternate Drug. Additive bradycardia effect may result in syncope.
- sotalol
metoprolol and sotalol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- thioridazine
metoprolol, thioridazine. Either increases levels of the other by decreasing metabolism. Contraindicated. Not all beta blockers share this interaction (e.g., atenolol, nadolol, sotalol do not interact).
- thiothixene
metoprolol, thiothixene. Either increases levels of the other by decreasing metabolism. Contraindicated. Not all beta blockers share this interaction (e.g., atenolol, nadolol, sotalol do not interact).
- timolol
metoprolol and timolol both increase anti-hypertensive channel blocking. Avoid or Use Alternate Drug.
- verapamil
verapamil, metoprolol. Either increases toxicity of the other by unspecified interaction mechanism. Avoid or Use Alternate Drug. Can increase risk of bradycardia.
Monitor Closely (204)
- abiraterone
abiraterone increases levels of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Avoid coadministration of abiraterone with substrates of CYP2D6. If alternative therapy cannot be used, exercise caution and consider a dose reduction of the CYP2D6 substrate.
- acebutolol
acebutolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- aceclofenac
metoprolol and aceclofenac both increase serum potassium. Use Caution/Monitor.
aceclofenac decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - acemetacin
metoprolol and acemetacin both increase serum potassium. Use Caution/Monitor.
acemetacin decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - albuterol
metoprolol increases and albuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of albuterol by pharmacodynamic antagonism. Use Caution/Monitor. - aldesleukin
aldesleukin increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- alfuzosin
alfuzosin and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- aluminum hydroxide
aluminum hydroxide decreases levels of metoprolol by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Separate by 2 hours.
- amifostine
amifostine, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Coadministration with blood pressure lowering agents may increase the risk and severity of hypotension associated with amifostine. When amifostine is used at chemotherapeutic doses, withhold blood pressure lowering medications for 24 hr prior to amifostine; if blood pressure lowering medication cannot be withheld, do not administer amifostine.
- amiloride
metoprolol and amiloride both increase serum potassium. Modify Therapy/Monitor Closely.
- amiodarone
amiodarone will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Monitor cardiac function carefully and observe for signs of bradycardia or heart block when amiodarone and a beta adrenergic blocker are coadministered. Amiodarone should be used with caution in patients receiving a beta adrenergic blocker, particularly if there is suspicion of underlying dysfunction of the sinus node, such as bradycardia or sick sinus syndrome, or if there is partial AV block.
amiodarone, metoprolol. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of cardiotoxicity with bradycardia. - amobarbital
amobarbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of amobarbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- arformoterol
metoprolol increases and arformoterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of arformoterol by pharmacodynamic antagonism. Use Caution/Monitor. - asenapine
asenapine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
asenapine and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely. - aspirin
metoprolol and aspirin both increase serum potassium. Use Caution/Monitor.
aspirin decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - aspirin rectal
metoprolol and aspirin rectal both increase serum potassium. Use Caution/Monitor.
aspirin rectal decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - aspirin/citric acid/sodium bicarbonate
aspirin/citric acid/sodium bicarbonate decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis.
metoprolol and aspirin/citric acid/sodium bicarbonate both increase serum potassium. Use Caution/Monitor. - atazanavir
atazanavir increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of hypotension, bradycardia, AV block, and prolonged PR interval. Consider lowering beta blocker dose.
- atenolol
atenolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- avanafil
avanafil increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- bendroflumethiazide
metoprolol increases and bendroflumethiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- betaxolol
betaxolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- bismuth subsalicylate
bismuth subsalicylate, metoprolol. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Blockage of renal prostaglandin synthesis; may cause severe hypertension.
- bisoprolol
bisoprolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- bretylium
metoprolol, bretylium. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Each drug may cause hypotension.
- bumetanide
metoprolol increases and bumetanide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- bupropion
bupropion will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- butabarbital
butabarbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of butabarbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- butalbital
butalbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of butalbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- calcium acetate
calcium acetate decreases effects of metoprolol by unspecified interaction mechanism. Use Caution/Monitor.
- calcium carbonate
calcium carbonate decreases effects of metoprolol by unspecified interaction mechanism. Use Caution/Monitor.
calcium carbonate decreases levels of metoprolol by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Separate by 2 hours. - calcium chloride
calcium chloride decreases effects of metoprolol by unspecified interaction mechanism. Use Caution/Monitor.
- calcium citrate
calcium citrate decreases effects of metoprolol by unspecified interaction mechanism. Use Caution/Monitor.
- calcium gluconate
calcium gluconate decreases effects of metoprolol by unspecified interaction mechanism. Use Caution/Monitor.
- candesartan
candesartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, candesartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - carbenoxolone
metoprolol increases and carbenoxolone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- carbidopa
carbidopa increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Therapy with carbidopa, given with or without levodopa or carbidopa-levodopa combination products, is started, dosage adjustment of the antihypertensive drug may be required.
- carvedilol
carvedilol and metoprolol both increase serum potassium. Use Caution/Monitor.
- celecoxib
celecoxib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
metoprolol and celecoxib both increase serum potassium. Use Caution/Monitor.
celecoxib decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - celiprolol
celiprolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- chloroquine
chloroquine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- chlorothiazide
metoprolol increases and chlorothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- chlorthalidone
metoprolol increases and chlorthalidone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- choline magnesium trisalicylate
metoprolol and choline magnesium trisalicylate both increase serum potassium. Use Caution/Monitor.
choline magnesium trisalicylate decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - cimetidine
cimetidine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- citalopram
citalopram increases levels of metoprolol by decreasing metabolism. Use Caution/Monitor. Increased metoprolol plasma levels have been associated with decreased cardioselectivity.
- clevidipine
metoprolol and clevidipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- clonidine
metoprolol, clonidine. Mechanism: pharmacodynamic synergism. Modify Therapy/Monitor Closely. Selective beta blocker administration during withdrawal from centrally acting alpha agonists may result in rebound hypertension.
clonidine, metoprolol. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Additive sympatholytic action may worsen sinus node dysfunction and atrioventricular (AV) block. - cobicistat
cobicistat will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- cyclopenthiazide
metoprolol increases and cyclopenthiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- darifenacin
darifenacin will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- darunavir
darunavir will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- dasiglucagon
metoprolol decreases effects of dasiglucagon by unknown mechanism. Use Caution/Monitor. Dasiglucagon may stimulate catecholamine release; whereas beta blockers may inhibit catecholamines released in response to dasiglucagon. Coadministration may also transiently increase pulse and BP.
- desflurane
desflurane, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- desvenlafaxine
desvenlafaxine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Desvenlafaxine inhibits CYP2D6; with higher desvenlafaxine doses (ie, 400 mg) decrease the CYP2D6 substrate dose by up to 50%; no dosage adjustment needed with desvenlafaxine doses <100 mg
- diclofenac
metoprolol and diclofenac both increase serum potassium. Use Caution/Monitor.
diclofenac decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - diflunisal
metoprolol and diflunisal both increase serum potassium. Use Caution/Monitor.
diflunisal decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - digoxin
metoprolol and digoxin both increase serum potassium. Use Caution/Monitor.
metoprolol increases effects of digoxin by pharmacodynamic synergism. Use Caution/Monitor. Enhanced bradycardia. - diltiazem
metoprolol and diltiazem both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- diphenhydramine
diphenhydramine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- dobutamine
metoprolol increases and dobutamine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of dobutamine by pharmacodynamic antagonism. Use Caution/Monitor. - dopexamine
metoprolol increases and dopexamine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of dopexamine by pharmacodynamic antagonism. Use Caution/Monitor. - doxazosin
doxazosin and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- dronedarone
dronedarone will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- drospirenone
metoprolol and drospirenone both increase serum potassium. Modify Therapy/Monitor Closely.
- duloxetine
duloxetine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- eliglustat
eliglustat increases levels of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Monitor therapeutic drug concentrations, as indicated, or consider reducing the dosage of the concomitant drug and titrate to clinical effect.
- ephedrine
metoprolol increases and ephedrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of ephedrine by pharmacodynamic antagonism. Use Caution/Monitor. - epinephrine
metoprolol increases and epinephrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of epinephrine by pharmacodynamic antagonism. Use Caution/Monitor. - epinephrine racemic
metoprolol increases and epinephrine racemic decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of epinephrine racemic by pharmacodynamic antagonism. Use Caution/Monitor. - eprosartan
eprosartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, eprosartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - esmolol
esmolol and metoprolol both increase serum potassium. Use Caution/Monitor.
- ethacrynic acid
metoprolol increases and ethacrynic acid decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- ether
metoprolol, ether. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Both beta blockers and ether depress the myocardium; consider lowering beta blocker dose if ether used for anesthesia.
- etodolac
metoprolol and etodolac both increase serum potassium. Use Caution/Monitor.
etodolac decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - etomidate
etomidate, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- etrasimod
etrasimod, metoprolol. pharmacodynamic synergism. Use Caution/Monitor. Transient decrease in heart rate and AV conduction delays may occur when initiating etrasimod. Concomitant use of etrasimod in patients receiving stable beta-blocker treatment did not result in additive effects on heart rate reduction. However, risk of additive heart rate reduction following initiation of beta-blocker therapy with stable etrasimod treatment or concomitant use with other drugs that may decrease heart rate is unknown. .
- fedratinib
fedratinib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Adjust dose of drugs that are CYP2D6 substrates as necessary.
- felodipine
metoprolol and felodipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- fenbufen
metoprolol and fenbufen both increase serum potassium. Use Caution/Monitor.
- fenoprofen
metoprolol and fenoprofen both increase serum potassium. Use Caution/Monitor.
fenoprofen decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - fingolimod
metoprolol increases effects of fingolimod by pharmacodynamic synergism. Use Caution/Monitor. Both medications decrease heart rate. Monitor patients on concomitant therapy, particularly in the first 6 hours after fingolimod is initiated or after a treatment interruption of at least two weeks, for bradycardia and atrioventricular block. To identify underlying risk factors of bradycardia and AV block, obtain a new or recent ECG in patients using beta-blockers prior to starting fingolimod.
- flurbiprofen
metoprolol and flurbiprofen both increase serum potassium. Use Caution/Monitor.
flurbiprofen decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - formoterol
metoprolol increases and formoterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of formoterol by pharmacodynamic antagonism. Use Caution/Monitor. - furosemide
metoprolol increases and furosemide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- gentamicin
metoprolol increases and gentamicin decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- glucagon
glucagon decreases toxicity of metoprolol by sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Use Caution/Monitor. Coadministration of glucagon with beta-blockers may have transiently increased pulse and blood pressure.
- glucagon intranasal
glucagon intranasal decreases toxicity of metoprolol by sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Use Caution/Monitor. Coadministration of glucagon with beta-blockers may have transiently increased pulse and blood pressure.
- haloperidol
haloperidol will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- hydralazine
hydralazine increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Additive hypotensive effects.
- hydrochlorothiazide
metoprolol increases and hydrochlorothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
hydrochlorothiazide, metoprolol. Either increases toxicity of the other by Other (see comment). Modify Therapy/Monitor Closely. Comment: May cause idiosyncratic reaction, resulting in acute transient myopia and acute angle-closure glaucoma, which can lead to permanent vision loss. - ibuprofen
metoprolol and ibuprofen both increase serum potassium. Use Caution/Monitor.
ibuprofen decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - ibuprofen IV
ibuprofen IV decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis.
metoprolol and ibuprofen IV both increase serum potassium. Use Caution/Monitor. - imatinib
imatinib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- indacaterol, inhaled
indacaterol, inhaled, metoprolol. Other (see comment). Use Caution/Monitor. Comment: Beta-blockers and indacaterol may interfere with the effect of each other when administered concurrently. Beta-blockers may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. However, under certain circumstances, e.g. as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
- indapamide
metoprolol increases and indapamide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- indomethacin
metoprolol and indomethacin both increase serum potassium. Use Caution/Monitor.
indomethacin decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - insulin degludec
metoprolol, insulin degludec. Other (see comment). Modify Therapy/Monitor Closely. Comment: Beta-blockers may either increase or decrease the blood glucose lowering effect of insulin; beta-blockers can prolong hypoglycemia (interference with glycogenolysis) or cause hyperglycemia (insulin secretion inhibited).
- insulin degludec/insulin aspart
metoprolol, insulin degludec/insulin aspart. Other (see comment). Modify Therapy/Monitor Closely. Comment: Beta-blockers may either increase or decrease the blood glucose lowering effect of insulin; beta-blockers can prolong hypoglycemia (interference with glycogenolysis) or cause hyperglycemia (insulin secretion inhibited).
- insulin inhaled
metoprolol, insulin inhaled. Other (see comment). Modify Therapy/Monitor Closely. Comment: Beta-blockers may either increase or decrease the blood glucose lowering effect of insulin; beta-blockers can prolong hypoglycemia (interference with glycogenolysis) or cause hyperglycemia (insulin secretion inhibited).
- irbesartan
irbesartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, irbesartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - isoproterenol
metoprolol increases and isoproterenol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of isoproterenol by pharmacodynamic antagonism. Use Caution/Monitor. - isradipine
metoprolol and isradipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- ivabradine
ivabradine, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Most patients receiving ivabradine will also be treated with a beta-blocker. The risk of bradycardia increases with coadministration of drugs that slow heart rate (eg, digoxin, amiodarone, beta-blockers). Monitor heart rate in patients taking ivabradine with other negative chronotropes.
- ketamine
ketamine, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- ketoprofen
metoprolol and ketoprofen both increase serum potassium. Use Caution/Monitor.
ketoprofen decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - ketorolac
metoprolol and ketorolac both increase serum potassium. Use Caution/Monitor.
ketorolac decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - ketorolac intranasal
metoprolol and ketorolac intranasal both increase serum potassium. Use Caution/Monitor.
ketorolac intranasal decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - labetalol
labetalol and metoprolol both increase serum potassium. Use Caution/Monitor.
- levalbuterol
metoprolol increases and levalbuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of levalbuterol by pharmacodynamic antagonism. Use Caution/Monitor. - levodopa
levodopa increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Consider decreasing dosage of antihypertensive agent.
- lorcaserin
lorcaserin will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- lornoxicam
metoprolol and lornoxicam both increase serum potassium. Use Caution/Monitor.
lornoxicam decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - losartan
losartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, losartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - lurasidone
lurasidone increases effects of metoprolol by Other (see comment). Use Caution/Monitor. Comment: Potential for increased risk of hypotension with concurrent use. Monitor blood pressure and adjust dose of antihypertensive agent as needed.
- maraviroc
maraviroc will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- marijuana
marijuana will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- meclofenamate
meclofenamate decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis.
metoprolol and meclofenamate both increase serum potassium. Use Caution/Monitor. - mefenamic acid
metoprolol and mefenamic acid both increase serum potassium. Use Caution/Monitor.
mefenamic acid decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - mefloquine
mefloquine increases levels of metoprolol by decreasing metabolism. Use Caution/Monitor. Risk of arrhythmia.
- meloxicam
metoprolol and meloxicam both increase serum potassium. Use Caution/Monitor.
meloxicam decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - metaproterenol
metoprolol increases and metaproterenol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of metaproterenol by pharmacodynamic antagonism. Use Caution/Monitor. - methyclothiazide
metoprolol increases and methyclothiazide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor. .
- metolazone
metoprolol increases and metolazone decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- mirabegron
mirabegron will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- moxisylyte
moxisylyte and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- nabumetone
metoprolol and nabumetone both increase serum potassium. Use Caution/Monitor.
nabumetone decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - nadolol
metoprolol and nadolol both increase serum potassium. Use Caution/Monitor.
- naproxen
metoprolol and naproxen both increase serum potassium. Use Caution/Monitor.
naproxen decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - nebivolol
metoprolol and nebivolol both increase serum potassium. Use Caution/Monitor.
- nicardipine
metoprolol and nicardipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- nifedipine
metoprolol and nifedipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- nilotinib
nilotinib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- nisoldipine
metoprolol and nisoldipine both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- nitroglycerin rectal
nitroglycerin rectal, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Beta-blockers blunt the reflex tachycardia produced by nitroglycerin without preventing its hypotensive effects. If beta-blockers are used with nitroglycerin in patients with angina pectoris, additional hypotensive effects may occur.
- norepinephrine
metoprolol increases and norepinephrine decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of norepinephrine by pharmacodynamic antagonism. Use Caution/Monitor. - olanzapine/samidorphan
olanzapine/samidorphan increases effects of metoprolol by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Monitor blood pressure and reduce antihypertensive drug dosage in accordance with its product labeling.
- olmesartan
olmesartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, olmesartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - oxaprozin
metoprolol and oxaprozin both increase serum potassium. Use Caution/Monitor.
oxaprozin decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - oxymetazoline topical
oxymetazoline topical increases and metoprolol decreases sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- panobinostat
panobinostat will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Panobinostat can increase the levels and effects of sensitive CYP2D6 substrates or those with a narrow therapeutic index CYP2D6.
- parecoxib
parecoxib will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
metoprolol and parecoxib both increase serum potassium. Use Caution/Monitor.
parecoxib decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - peginterferon alfa 2b
peginterferon alfa 2b, metoprolol. Other (see comment). Use Caution/Monitor. Comment: When patients are administered peginterferon alpha-2b with CYP2D6 substrates, the therapeutic effect of these drugs may be altered. Peginterferon alpha-2b may increase or decrease levels of CYP2D6 substrate.
- penbutolol
metoprolol and penbutolol both increase serum potassium. Use Caution/Monitor.
- pentobarbital
pentobarbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of pentobarbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- perphenazine
perphenazine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- phenobarbital
phenobarbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of phenobarbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- phenoxybenzamine
phenoxybenzamine and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- phentolamine
phentolamine and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- pindolol
metoprolol and pindolol both increase serum potassium. Use Caution/Monitor.
- pirbuterol
metoprolol increases and pirbuterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of pirbuterol by pharmacodynamic antagonism. Use Caution/Monitor. - piroxicam
metoprolol and piroxicam both increase serum potassium. Use Caution/Monitor.
piroxicam decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - ponesimod
ponesimod and metoprolol both increase pharmacodynamic synergism. Use Caution/Monitor. Beta-blockers may have additive effects on lowering HR. Consider resting HR before initiating ponesimod in patients on stable dose of beta-blocker. Refer to the ponesimod prescribing information for more dosing information.
- potassium acid phosphate
metoprolol and potassium acid phosphate both increase serum potassium. Modify Therapy/Monitor Closely.
- potassium chloride
metoprolol and potassium chloride both increase serum potassium. Modify Therapy/Monitor Closely.
- potassium citrate
metoprolol and potassium citrate both increase serum potassium. Modify Therapy/Monitor Closely.
- prazosin
prazosin and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- primidone
primidone decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of primidone. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- propafenone
propafenone will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. If concurrent therapy is required, monitor cardiac function carefully, particularly blood pressure. A dosage adjustment for the beta blocker may be required.
- propofol
propofol, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- propranolol
metoprolol and propranolol both increase serum potassium. Use Caution/Monitor.
- quinacrine
quinacrine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- ranolazine
ranolazine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- rifabutin
rifabutin decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Enzyme induction effect may continue for up to 3-4 weeks.
- rifampin
rifampin decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor.
- rifapentine
rifapentine decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor.
- ritonavir
ritonavir will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- rolapitant
rolapitant will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Rolapitant may increase plasma concentrations of CYP2D6 substrates for at least 28 days following rolapitant administration.
- sacubitril/valsartan
sacubitril/valsartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, sacubitril/valsartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - salicylates (non-asa)
metoprolol and salicylates (non-asa) both increase serum potassium. Use Caution/Monitor.
salicylates (non-asa) decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - salmeterol
metoprolol increases and salmeterol decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol decreases effects of salmeterol by pharmacodynamic antagonism. Use Caution/Monitor. - salsalate
metoprolol and salsalate both increase serum potassium. Use Caution/Monitor.
salsalate decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - saquinavir
saquinavir, metoprolol. Either increases toxicity of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Use alternatives if available. Increased risk of PR prolongation and cardiac arrhythmias.
- secobarbital
secobarbital decreases levels of metoprolol by increasing metabolism. Use Caution/Monitor. Consider a higher beta-blocker dose during coadministration of secobarbital. Atenolol, sotalol, nadolol less likely to be affected than other beta blockers.
- sertraline
sertraline will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- sevoflurane
sevoflurane, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- sildenafil
metoprolol increases effects of sildenafil by additive vasodilation. Use Caution/Monitor. Sildenafil has systemic vasodilatory properties and may further lower blood pressure in patients taking antihypertensive medications. Monitor blood pressure response to sildenafil in patients receiving concurrent blood pressure lowering therapy.
- silodosin
silodosin and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- siponimod
siponimod, metoprolol. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Caution when siponimod is initiated in patients receiving beta-blocker treatment because of additive effects on lowering heart rate. Temporary interruption of beta-blocker may be needed before initiating siponimod. Beta-blocker treatment can be initiated in patients receiving stable doses of siponimod.
- sodium bicarbonate
sodium bicarbonate decreases levels of metoprolol by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Separate by 2 hours.
- sodium citrate/citric acid
sodium citrate/citric acid decreases levels of metoprolol by inhibition of GI absorption. Applies only to oral form of both agents. Use Caution/Monitor. Separate by 2 hours.
- sotalol
metoprolol and sotalol both increase serum potassium. Use Caution/Monitor.
- spironolactone
metoprolol and spironolactone both increase serum potassium. Modify Therapy/Monitor Closely.
- succinylcholine
metoprolol and succinylcholine both increase serum potassium. Use Caution/Monitor.
- sulfasalazine
metoprolol and sulfasalazine both increase serum potassium. Use Caution/Monitor.
sulfasalazine decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - sulindac
metoprolol and sulindac both increase serum potassium. Use Caution/Monitor.
sulindac decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - tadalafil
tadalafil increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor. Risk of hypotension.
- telmisartan
telmisartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, telmisartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - terazosin
terazosin and metoprolol both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- terbinafine
terbinafine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Assess need to reduce dose of CYP2D6-metabolized drug.
- terbutaline
metoprolol increases and terbutaline decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
metoprolol increases effects of terbutaline by pharmacodynamic synergism. Use Caution/Monitor.
metoprolol decreases effects of terbutaline by pharmacodynamic antagonism. Use Caution/Monitor. - theophylline
metoprolol, theophylline. Other (see comment). Use Caution/Monitor. Comment: Beta blockers (esp. non selective) antagonize theophylline effects, while at the same time increasing theophylline levels and toxicity (mechanism: decreased theophylline metabolism). Smoking increases risk of interaction.
- thioridazine
thioridazine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- timolol
metoprolol and timolol both increase serum potassium. Use Caution/Monitor.
- tipranavir
tipranavir will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- tolfenamic acid
metoprolol and tolfenamic acid both increase serum potassium. Use Caution/Monitor.
tolfenamic acid decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - tolmetin
metoprolol and tolmetin both increase serum potassium. Use Caution/Monitor.
tolmetin decreases effects of metoprolol by pharmacodynamic antagonism. Use Caution/Monitor. Long term (>1 wk) NSAID use. NSAIDs decrease prostaglandin synthesis. - tolvaptan
metoprolol and tolvaptan both increase serum potassium. Use Caution/Monitor.
- torsemide
metoprolol increases and torsemide decreases serum potassium. Effect of interaction is not clear, use caution. Use Caution/Monitor.
- triamterene
metoprolol and triamterene both increase serum potassium. Modify Therapy/Monitor Closely.
- valsartan
valsartan and metoprolol both increase serum potassium. Use Caution/Monitor.
metoprolol, valsartan. Mechanism: pharmacodynamic synergism. Use Caution/Monitor. Risk of fetal compromise if given during pregnancy. - venlafaxine
venlafaxine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- verapamil
metoprolol and verapamil both increase anti-hypertensive channel blocking. Modify Therapy/Monitor Closely.
- xipamide
xipamide increases effects of metoprolol by pharmacodynamic synergism. Use Caution/Monitor.
Minor (32)
- adenosine
metoprolol, adenosine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Bradycardia.
- agrimony
agrimony increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- antipyrine
metoprolol increases levels of antipyrine by decreasing metabolism. Minor/Significance Unknown.
- brimonidine
brimonidine increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- cevimeline
cevimeline increases effects of metoprolol by unspecified interaction mechanism. Minor/Significance Unknown.
- ciprofloxacin
ciprofloxacin increases levels of metoprolol by decreasing metabolism. Minor/Significance Unknown. Ciprofloxacin may increase metoprolol plasma concentrations however mechanism is unknown. Further clinical evidence is needed but it may be appropriate to monitor patients during concomitant therapy with ciprofloxacin.
- cocaine topical
metoprolol increases effects of cocaine topical by pharmacodynamic synergism. Minor/Significance Unknown. Risk of angina.
- cornsilk
cornsilk increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- diazepam
metoprolol increases effects of diazepam by decreasing metabolism. Minor/Significance Unknown.
- dihydroergotamine
dihydroergotamine, metoprolol. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Additive vasospasm.
- dihydroergotamine intranasal
dihydroergotamine intranasal, metoprolol. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Additive vasospasm.
- dipyridamole
dipyridamole, metoprolol. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Risk of bradycardia.
- escitalopram
escitalopram increases levels of metoprolol by decreasing metabolism. Minor/Significance Unknown.
- fenoldopam
fenoldopam increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown. Additive hypotensive effects.
- forskolin
forskolin increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- guanfacine
metoprolol, guanfacine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Selective beta blocker administration during withdrawal from centrally acting alpha agonists may result in rebound hypertension.
- imaging agents (gadolinium)
metoprolol, imaging agents (gadolinium). Mechanism: unknown. Minor/Significance Unknown. Increased risk of anaphylaxis from contrast media.
- levobetaxolol
levobetaxolol increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- maitake
maitake increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- metipranolol ophthalmic
metipranolol ophthalmic increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- neostigmine
metoprolol, neostigmine. Either increases effects of the other by pharmacodynamic synergism. Minor/Significance Unknown. Additive bradycardia.
- noni juice
metoprolol and noni juice both increase serum potassium. Minor/Significance Unknown.
- octacosanol
octacosanol increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- oxazepam
metoprolol increases effects of oxazepam by decreasing metabolism. Minor/Significance Unknown.
- patiromer
patiromer, metoprolol. cation binding in GI tract. Minor/Significance Unknown. No observed clinically important interaction. No separation of dosing required.
- physostigmine
metoprolol, physostigmine. Either increases effects of the other by pharmacodynamic synergism. Minor/Significance Unknown. Additive bradycardia.
- pilocarpine
pilocarpine increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- reishi
reishi increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- shepherd's purse
shepherd's purse, metoprolol. Other (see comment). Minor/Significance Unknown. Comment: Theoretically, shepherd's purse may interfere with BP control.
- tizanidine
tizanidine increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown. Risk of hypotension.
- treprostinil
treprostinil increases effects of metoprolol by pharmacodynamic synergism. Minor/Significance Unknown.
- yohimbe
metoprolol decreases toxicity of yohimbe by pharmacodynamic antagonism. Minor/Significance Unknown.
Adverse Effects
1-10%
Dizziness (10%)
Headache (10%)
Tiredness (10%)
Depression (5%)
Diarrhea (5%)
Pruritus (5%)
Bradycardia (9%)
Rash (5%)
Dyspnea (1-3%)
Cold extremities (1%)
Constipation (1%)
Dyspepsia (1%)
Heart failure (1%)
Hypotension (1%)
Nausea (1%)
Flatulence (1%)
Heartburn (1%)
Xerostomia (1%)
Wheezing (1%)
Bronchospasm (1%)
Frequency Not Defined
Decreased exercise tolerance
Raynaud phenomenon
Increased triglyceride levels and insulin resistance, decreased high-density lipoprotein (HDL) levels
Postmarketing reports
Anxiety/nervousness
Hallucinations
Paresthesia
Hepatitis
Vomiting
Arthralgia
Male impotence
Reversible alopecia
Agranulocytosis
Dry eyes
Worsening of psoriasis
Pyronie’s disease
Sweating
Photosensitivity
Taste disturbance
Warnings
Contraindications
Hypersensitivity
Lopressor
- Hypertension and angina: Sinus bradycardia, 2°/3° heart block, cardiogenic shock, sick sinus syndrome (unless permanent pacemaker in place), severe peripheral vascular disease, pheochromocytoma
- Myocardial infarction: Severe sinus bradycardia, heart rate <45 beats/min, systolic BP <100 mmHg, significant first-degree heart block ((PR interval at least 0.24 seconds), 2°/3° heart block, moderate-to-severe cardiac failure
Toprol XL
- Second- and third-degree heart block, deompensated heart failure, sick sinus syndrome (except in patients with functioning artificial pacemaker), severe bradycardia, cardiogenic shock
Kapspargo Sprinkle
- Severe bradycardia, second or third degree heart block, cardiogenic shock, decompensated heart failure, sick sinus syndrome (unless a permanent pacemaker is in place), and in patients who are hypersensitive to any component of this product
Cautions
Use with caution in cerebrovascular insufficiency, CHF, cardiomegaly, myasthenia gravis, hyperthyroidism or thyrotoxicosis (may mask signs or symptoms), liver disease, renal impairment, peripheral vascular disease, psoriasis (may cause exacerbation of psoriasis)
May exacerbate bronchospastic disease; monitor closely
Beta-blockers can cause myocardial depression and may precipitate heart failure and cardiogenic shock
Sudden discontinuance can exacerbate angina and lead to MI and ventricular arrhythmias in patients with CAD
Worsening cardiac failure may occur during up-titration of metoprolol succinate; if such symptoms occur, increase diuretics and restore clinical stability before advancing the dose of metoprolol succinate; it may be necessary to lower the dose of metoprolol succinate or temporarily discontinue it
Bradycardia, including sinus pause, heart block, and cardiac arrest, has been reported; patients with 1° atrioventricular block, sinus node dysfunction, or conduction disorders may be at increased risk; monitor heart rate in patients receiving metoprolol succinate; if severe bradycardia develops, reduce or stop metoprolol succinate
Increased risk of stroke after surgery
Beta-blockers may prevent early warning signs of hypoglycemia, such as tachycardia, and increase risk for severe or prolonged hypoglycemia at any time during treatment, especially in patients with diabetes mellitus or children and patients who are fasting (ie, surgery, not eating regularly, or are vomiting); if severe hypoglycemia occurs, patients should be instructed to seek emergency treatment
Avoid starting high-dose regimen of extended-release metoprolol in patients undergoing noncardiac surgery; use in patients with cardiovascular risk factors is associated with bradycardia, hypotension, stroke, and death
Long-term beta blockers should not be routinely withdrawn before major surgery; however, impaired ability of the heart to respond to reflex adrenergic stimuli may augment risks of general anesthesia and surgical procedures
Metoprolol loses beta-receptor selectivity at high doses and in poor metabolizers
If drug is administered for tachycardia secondary to pheochromocytoma, it should be given in combination with an alpha blocker (which should be started before metoprolol is started)
While taking beta blockers, patients with history of severe anaphylactic reaction to variety of allergens may be more reactive to repeated challenge
Extended release tablet should not be withdrawn routinely prior to major surgery
Hydrochlorothiazide, can cause an idiosyncratic reaction, resulting in acute transient myopia and acute angle-closure glaucoma, which can lead to permanent vision loss if not treated; discontinue hydrochlorothiazide as rapidly as possible if symptoms occur; prompt medical or surgical treatments may need to be considered if intraocular pressure remains uncontrolled; risk factors for developing acute angle-closure glaucoma may include history of sulfonamide or penicillin allergy
Caution in patients with history of psychiatric illness; may cause or exacerbate CNS depression
Beta-blockers can precipitate or aggravate symptoms of arterial insufficiency in patients with peripheral vascular disease
Drug interactions overview
- Catecholamine depleting drugs (eg, reserpine, monoamine oxidase (MAO) inhibitors) may have an additive effect when given with beta-blocking agents; monitor when coadministration with catecholamine depleting drugs for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension
- While taking beta-blockers, patients with a history of severe anaphylactic reactions to a variety of allergens may be more reactive to repeated challenge and may be unresponsive to the usual doses of epinephrine used to treat an allergic reaction
- Drugs that are strong inhibitors of CYP2D6, such as quinidine, fluoxetine, paroxetine, and propafenone, were shown to double metoprolol concentrations; no information about moderate or weak inhibitors, but are likely to increase metoprolol concentration; closely monitor patients when the combination cannot be avoided
- Digitalis glycosides, clonidine, diltiazem and verapamil slow atrioventricular conduction and decrease heart rate
- Concomitant administration of hydralazine may inhibit presystemic metabolism of metoprolol leading to increased concentrations of metoprolol
- Concomitant use with beta blockers can increase the risk of bradycardia; if clonidine and a beta blocker, such as metoprolol are coadministered, withdraw the beta-blocker several days before the gradual withdrawal of clonidine because beta-blockers may exacerbate the rebound hypertension that can follow the withdrawal of clonidine
- If replacing clonidine by beta-blocker therapy, delay introduction of beta-blockers for several days after clonidine administration has stopped
- Metoprolol succinate is released faster from Kapspargo Sprinkle in the presence of alcohol; may increase the risk for adverse events associated with Kapspargo Sprinkle
- Avoid alcohol consumption
Pregnancy & Lactation
Pregnancy
Untreated hypertension and heart failure during pregnancy increases maternal risk for pre-eclampsia, gestational diabetes, premature delivery, and delivery complications (eg, need for cesarean section, and post-partum hemorrhage)
Hypertension increases fetal risk for intrauterine growth restriction and intrauterine death; pregnant women with hypertension should be carefully monitored and managed accordingly
Stroke volume and heart rate increase during pregnancy, increasing cardiac output, especially during first trimester; there is a risk for preterm birth with pregnant women with chronic heart failure in 3rd trimester of pregnancy
Available data from published observational studies have not demonstrated a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes with metoprolol use during pregnancy
However, there are inconsistent reports of intrauterine growth restriction, preterm birth, and perinatal mortality with maternal use of beta blockers, including metoprolol, during pregnancy
Metoprolol crosses placenta; neonates born to mothers who are receiving metoprolol during pregnancy, may be at risk for hypotension, hypoglycemia, bradycardia, and respiratory depression; observe neonates and manage accordingly
Females and males of reproductive potential
- Based on published literature, beta blockers (including metoprolol) may cause erectile dysfunction and inhibit sperm motility
- No evidence of impaired fertility due to metoprolol observed in rats
Animal data
- Lopressor has been shown to increase postimplantation loss and decrease neonatal survival in rats at doses of 500 mg/kg/day, approximately 24 times the daily human dose of 200 mg, in a 60-kg patient when based on surface area (mg/m2)
- Distribution studies in mice confirm exposure of the fetus when Lopressor is administered to the pregnant animal
- These limited animal studies do not indicate direct or indirect harmful effects with respect to teratogenicity
Lactation
Limited available data from published literature report that metoprolol is present in human milk; the estimated daily infant dose of metoprolol received from breastmilk ranges from 0.05 mg to less than 1 mg; the estimated relative infant dosage was 0.5% to 2% of the mother's weight-adjusted dosage; no adverse reactions of metoprolol on the breastfed infant have been identified; there is no information regarding the effects of metoprolol on milk production
Monitor breastfed infant for bradycardia and other symptoms of beta-blockade such as listlessness (hypoglycemia)
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
Blocks response to beta-adrenergic stimulation; cardioselective for beta1 receptors at low doses, with little or no effect on beta2 receptors
Absorption
Bioavailability: 40-50% (immediate-release) ; 65-77% (extended-release) relative to immediate release
Onset: 20 min (IV), when infused over 10 min; onset may be immediate, depending on clinical setting; 1-2 hr (PO)
Duration: 3-6 hr (PO); duration is dose-related; 24 hr (ER); 5-8 hr (IV)
Peak plasma time: 1.5-2 hr (immediate-release); 3.3 hr (extended-release)
Therapeutic range: 35-212 ng/mL
Distribution
Protein bound: 10%
Vd: 3.2-5.6 L/kg
Metabolism
Metabolized in liver by CYP2D6
Metabolites: Inactive
Elimination
Half-life: 3-4 hr (average); 7.5 hr (poor metabolizers); 2.8 hr (extensive metabolizers)
Excretion: Urine (95%)
Administration
IV Compatibilities
Solution: D5W, NS
Y-site: Abciximab, alteplase, argatroban, meperidine, morphine sulfate
IV Incompatibilities
Y-site: Amphotericin B cholesteryl sulfate
IV Administration
Give undiluted by direct injection
Oral Administration
Metoprolol tartrate: Take with or immediately after meals
Metoprolol succinate: Tablet should not be chewed or crushed
Kapspargo Sprinkle
- Swallow whole
- For patients unable to swallow an intact capsule, alternative administration options are available
Directions for use with soft food (applesauce, pudding, or yogurt)
- Open capsule and sprinkle contents soft food
- Contents of the capsules should be swallowed along with a small amount (teaspoonful) of soft food (such as applesauce, pudding, or yogurt)
- Drug/food mixture should be swallowed within 60 minutes and not stored for future use
Nasogastric tube administration
Kapspargo Sprinkle
- Open and add contents of capsule to an all plastic oral tip syringe and add 15 mL of water
- Gently shake the syringe for ~10 seconds
- Promptly deliver through a 12 French or larger nasogastric tube
- Ensure no granules are left in the syringe
- Rinse with additional water if needed
Storage
Do not freeze
Lopressor
- Tablets: Store at room temperature
- Unused vials: Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F); protect from light and heat
Kapspargo Sprinkle
- Store at 20- 25°C (68-77°F)
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| Kapspargo Sprinkle oral - | 100 mg capsule |  | |
| Toprol XL oral - | 25 mg tablet | 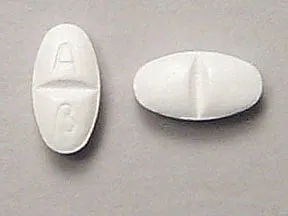 | |
| Toprol XL oral - | 50 mg tablet |  | |
| Toprol XL oral - | 200 mg tablet |  | |
| Toprol XL oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet | 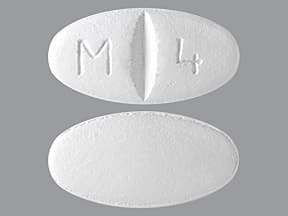 | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet | 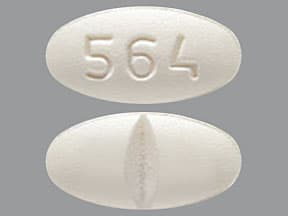 | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet | 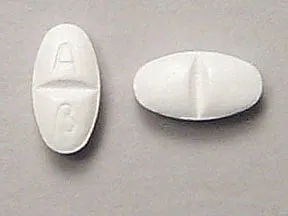 | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet | 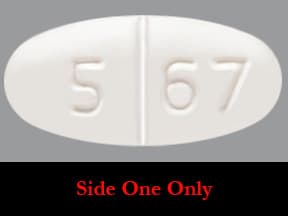 | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 100 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet | 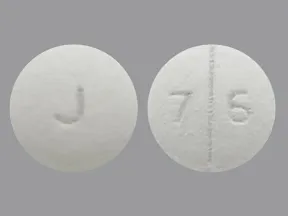 | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet | 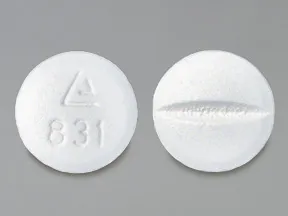 | |
| metoprolol succinate oral - | 25 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  | |
| metoprolol succinate oral - | 50 mg tablet |  | |
| metoprolol succinate oral - | 200 mg tablet |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
metoprolol succinate oral
METOPROLOL SUCCINATE EXTENDED-RELEASE TABLET - ORAL
(MET-oh-PROE-lol SUX-i-nate)
COMMON BRAND NAME(S): Toprol XL
WARNING: Do not stop taking this medication without consulting your doctor. Some conditions may become worse when you suddenly stop this drug. Some people who have suddenly stopped taking similar drugs have had chest pain, heart attack, and irregular heartbeat. If your doctor decides you should no longer use this drug, your doctor may direct you to gradually decrease your dose over 1 to 2 weeks.When gradually stopping this medication, it is recommended that you temporarily limit physical activity to decrease strain on the heart. Get medical help right away if you develop chest pain/tightness/pressure, chest pain spreading to the jaw/neck/arm, unusual sweating, trouble breathing, or fast/irregular heartbeat.
USES: This medication is a beta-blocker used to treat chest pain (angina), heart failure, and high blood pressure. Lowering high blood pressure helps prevent strokes, heart attacks, and kidney problems.This drug works by blocking the action of certain natural chemicals in your body (such as epinephrine) that affect the heart and blood vessels. This lowers heart rate, blood pressure, and strain on the heart.
HOW TO USE: See also Warning section.Take this medication by mouth as directed by your doctor, usually once daily. This medication may be taken with or without food.Do not crush or chew extended-release tablets. Doing so can release all of the drug at once, increasing the risk of side effects. Also, do not split extended-release tablets unless they have a score line and your doctor or pharmacist tells you to do so. Swallow the whole or split tablet without crushing or chewing.To reduce your risk of side effects, your doctor may direct you to start this medication at a low dose and gradually increase your dose. Follow your doctor's instructions carefully. The dosage is based on your medical condition and response to treatment.Use this medication regularly to get the most benefit from it. To help you remember, take it at the same time each day. Do not suddenly stop taking this medication without consulting your doctor. Your condition may become worse when the drug is suddenly stopped.For the treatment of high blood pressure, it may take several weeks before you get the full benefit of this drug. Keep taking this medication even if you feel well. Most people with high blood pressure do not feel sick.To prevent chest pain, a second heart attack, or migraine headaches, it is very important to take this medication regularly as prescribed. This drug should not be used to treat chest pain or migraines when they occur. Use other medications to relieve sudden attacks as directed by your doctor (for example, nitroglycerin tablets placed under the tongue for chest pain, "triptan" drugs such as sumatriptan for migraines). Consult your doctor or pharmacist for details.Tell your doctor if your condition does not get better or if it gets worse (for example, your blood pressure readings remain high or increase, your chest pain or migraines occur more often).
SIDE EFFECTS: See also Warning section.Drowsiness, dizziness, tiredness, diarrhea, and slow heartbeat may occur. Decreased sexual ability has been reported rarely. If any of these effects last or get worse, tell your doctor or pharmacist promptly.To reduce the risk of dizziness and lightheadedness, get up slowly when rising from a sitting or lying position.With some brands of this medication, an empty tablet shell may appear in your stool. This is harmless.This drug may reduce blood flow to your hands and feet, causing them to feel cold. Smoking may worsen this effect. Dress warmly and avoid tobacco use.Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Tell your doctor right away if you have any serious side effects, including: very slow heartbeat, fainting, blue fingers/toes, new or worsening symptoms of heart failure (such as shortness of breath, swelling ankles/feet, unusual tiredness, unusual/sudden weight gain), mental/mood changes (such as confusion, mood swings, depression).A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before taking metoprolol, tell your doctor or pharmacist if you are allergic to it; or to other beta-blockers (such as atenolol, propranolol); or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history, especially of: certain types of heart rhythm problems (such as a slow heartbeat, second- or third-degree atrioventricular block, sick sinus syndrome), breathing problems (such as asthma, chronic bronchitis, emphysema), liver disease, serious allergic reactions, including those needing treatment with epinephrine, blood circulation problems (such as Raynaud's disease, peripheral vascular disease), mental/mood disorders (such as depression), a certain muscle disease (myasthenia gravis).This drug may make you dizzy or drowsy. Alcohol or marijuana (cannabis) can make you more dizzy or drowsy. Do not drive, use machinery, or do anything that needs alertness until you can do it safely. Limit or avoid alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).This product may prevent the fast/pounding heartbeat you would usually feel when your blood sugar level falls too low (hypoglycemia). The risk is higher if you have diabetes, or are vomiting, fasting, or not eating regularly. Other symptoms of low blood sugar level, such as dizziness and sweating, are not affected by this drug.If you have diabetes, this product may make it harder to control your blood sugar levels. Check your blood sugar levels regularly as directed by your doctor. Tell your doctor right away if you have symptoms of high blood sugar such as increased thirst/urination. Your doctor may need to adjust your diabetes medication, exercise program, or diet.Children may be at greater risk for low blood sugar (hypoglycemia) while using this drug, especially if they are vomiting or not eating regularly. To help prevent low blood sugar, make sure children eat regularly. If your child cannot eat regularly, is vomiting, or has symptoms of low blood sugar (such as sweating, shaking), tell the doctor right away.During pregnancy, this medication should be used only when clearly needed. It may harm an unborn baby. Discuss the risks and benefits with your doctor.This drug passes into breast milk but is unlikely to harm a nursing infant. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.A product that may interact with this drug is: fingolimod.Other medications can affect the removal of metoprolol from your body, which may affect how metoprolol works. Examples include lumefantrine, propafenone, quinidine, SSRI antidepressants (such as fluoxetine, paroxetine), St. John's wort, among others.Some products have ingredients that could raise your heart rate or blood pressure or worsen your heart failure. Tell your pharmacist what products you are using, and ask how to use them safely (especially cough-and-cold products, diet aids, or NSAIDs such as ibuprofen/naproxen).
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: very slow heartbeat, severe dizziness, severe weakness, fainting, trouble breathing.
NOTES: Do not share this medication with others.Talk with your doctor about lifestyle changes that may help this medication work better (such as stress reduction programs, exercise, and dietary changes).Have your blood pressure and pulse (heart rate) checked regularly while taking this medication. Learn how to check your own blood pressure and pulse at home, and share the results with your doctor.Lab and/or medical tests (such as liver function tests) should be done while you are taking this medication. Consult your doctor for more details.
MISSED DOSE: If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
STORAGE: Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
MEDICAL ALERT: Your condition can cause complications in a medical emergency. For information about enrolling in MedicAlert, call 1-888-633-4298 (US) or 1-800-668-1507 (Canada).
Information last revised March 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.





