History
The hallmark feature of rheumatoid arthritis (RA) is persistent symmetric polyarthritis (synovitis) that affects the hands and feet, although any joint lined by a synovial membrane may be involved. The severity of RA may fluctuate over time, but chronic RA most commonly results in the progressive development of various degrees of joint destruction, deformity, and a significant decline in functional status. Extra-articular involvement of organs such as the skin, heart, lungs, and eyes can also be significant.
Juvenile idiopathic arthritis (JIA), sometimes referred to as juvenile rheumatoid arthritis (JRA), is the most common form of childhood arthritis. In most patients, the immunogenic associations, clinical pattern, and functional outcome of JIA are different from those of adult-onset RA.
Patients with RA may report difficulty performing activities of daily living (ADLs), such as dressing, standing, walking, personal hygiene, or use of their hands. In addition to articular deterioration, constitutional symptoms (eg, fatigue, malaise, morning stiffness, weight loss, and low-grade fever) may be present.
In most patients, RA has an insidious onset. It may begin with systemic features (eg, fever, malaise, arthralgias, and weakness) before the appearance of overt joint inflammation and swelling. A small percentage (approximately 10%) of patients have an abrupt onset with the acute development of synovitis and extra-articular manifestations. Spontaneous remission may occur but is uncommon, especially after the first 3-6 months.
Physical Examination
During the physical examination, it is important to assess for the following:
-
Stiffness
-
Tenderness
-
Pain on motion
-
Swelling
-
Deformity
-
Limitation of motion
-
Extra-articular manifestations
-
Rheumatoid nodules
Joint involvement is the characteristic feature of RA. In general, the small joints of the hands and feet are affected in a relatively symmetric distribution. In decreasing frequency, the metacarpophalangeal (MCP), wrist, proximal interphalangeal (PIP), knee, metatarsophalangeal (MTP), shoulder, ankle, cervical spine, hip, elbow, and temporomandibular joints are most commonly affected.
Affected joints show inflammation with swelling, tenderness, warmth, and decreased range of motion (ROM). Atrophy of the interosseous muscles of the hands is a typical early finding. Joint and tendon destruction may lead to deformities such as ulnar deviation, boutonniere and swan-neck deformities, hammer toes, and, occasionally, joint ankylosis.
Other commonly observed musculoskeletal manifestations include the following:
-
Tenosynovitis (defined as inflammation of the tendon and its enveloping tendon sheath) and associated tendon rupture due to tendon and ligament involvement, most commonly involving the fourth and fifth digital extensor tendons at the wrist
-
Periarticular osteoporosis due to localized inflammation
-
Generalized osteoporosis due to systemic chronic inflammation, immobility, or corticosteroid therapy
Most patients with RA have muscle atrophy from disuse, which is often secondary to joint inflammation.
Examination of upper extremities
Fingers
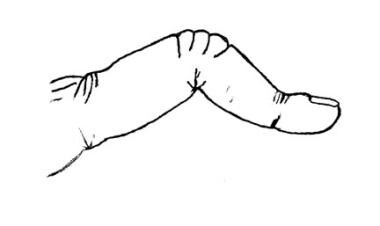
The boutonniere deformity (see the image below) describes nonreducible flexion at the PIP joint along with hyperextension of the distal interphalangeal (DIP) joint of the finger.
This deformity occurs as a result of synovitis stretching or rupturing the PIP joint through the central extensor tendon, with concomitant volar displacement of the lateral bands. When the lateral bands have subluxed far enough to pass the transverse axis of the joint, they become flexors of the PIP joint. Hyperextension of the DIP joint occurs as the tendons shorten with time. A compensatory and reducible hyperextension may occur at the MCP joint. Consequences of boutonniere deformity are loss of thumb mobility and pincher grasp.
Swan-neck deformity of the finger describes hyperextension at the PIP joint with flexion of the DIP joint (see the image below).
This deformity may be initiated either (a) by disruption of the extensor tendon at the DIP joint, with secondary shortening of the central extensor tendon and hyperextension of the PIP joint, or (b) by volar herniation of the PIP joint capsule due to weakening from chronic synovitis, with subsequent tightening of the lateral bands and central extensor tendon. The lateral bands may become shortened over time and lie dorsally, limiting PIP flexion and ineffectively extending the DIP joint.
Tightness of intrinsic muscles (eg, the interossei and lumbricals) may cause major declines in finger mobility. This tightness is ascertained on examination when the PIP joint cannot be flexed while the MCP joint is fully extended but can be flexed while the MCP is in flexion (Bunnell test); primary PIP joint pathology is evident with the MCP joint in either position. For accurate assessment, the phalanx must be aligned with the metacarpal; when ulnar deviation at the MCP joint exists, the intrinsic muscles on the ulnar side are slack, allowing more motion.
Flexor tenosynovitis of the fingers is common and suggests a poor prognosis. “Triggering” of the finger occurs when thickening or nodule formation of the tendon interacts with the concomitant tenosynovial proliferation, trapping the tendon in a flexed position (stenosing tenosynovitis). Tendon rupture may occur as a consequence of infiltrative synovitis in the digit or bony erosion of the tendon at the wrist (especially the flexor pollicis longus). See Trigger Finger.
Arthritis mutilans (sometimes called opera glass hands) results if destruction is severe and extensive, with dissolution of bone. In the small joints of the hands, the phalanges may shorten, and the joints may become grossly unstable. Pulling on the fingers during examination may lengthen the digit in a manner resembling the opening of opera glasses, or the joint may bend in unusual directions merely under the pull of gravity.
Metacarpophalangeal joints
Two typical deformities that alter the alignment of the palmar skeletal arches and the stability of the fingers may occur at the MCP joints: volar subluxation and ulnar deviation (see the image below).
 Rheumatoid arthritis. Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
Rheumatoid arthritis. Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
Most cases of ulnar deviation are accompanied by counterpoised radial deviation of the wrist, roughly proportional to the degree of ulnar deviation of the fingers. The volar plate is firmer and more substantial than other portions of the MCP joint capsule, thus effectively limiting extension and dorsal movement at the joint. The greater strength of the flexor muscles relative to the extensor muscles causes volar migration of the proximal phalanx after synovial-based inflammation has weakened ligament and tendon insertions about the MCP joint capsule.
Ulnar deviation occurs after synovitis has led to stretching and attenuation of the volar plate and collateral ligaments, allowing dislocation of the flexor tendon volarward and ulnarward. The supporting structures of the extensor tendons also may become attenuated or destroyed by synovial distention and invasion, loosening the tendons so that they no longer ride centrally and dorsally over the metacarpal head but move into the cleft between the MCP joints.
If the extensor tendon subluxation is beyond the transverse axis of the MCP joint, the tendon becomes a flexor at that joint, further limiting the active extension of the fingers.
Wrists
Multiple deformities may occur in the wrist. Disruption of the radioulnar joint with dorsal subluxation of the ulna (caput ulnae) as well as rotation of the carpus on the distal radius with an ulnarly translocated lunate are common. The combination of an ulnar drift of the fingers and carpal rotation is known as a zigzag deformity. Shortening of the carpal height (noted on radiographs), due in part to cartilage loss, is seen with rotational deformities.
Dorsal subluxation of the ulna often allows the ulnar styloid to be depressed volarly on examination, much as a piano key is depressed when played. It may lead to rupture of the extensor tendons of the little, ring, and long fingers because the end of the distal ulna is roughened secondary to erosion of bone and may abrade the tendons as they move during normal hand function, much as a rope is frayed when rubbed over a sharp rock (see the image below). This process is especially likely to lead to tendon rupture if tenosynovitis is present.
 Rheumatoid arthritis. Coronal, T1-weighted magnetic resonance imaging scan shows characteristic pannus and erosive changes in the wrist in a patient with active rheumatoid arthritis. Courtesy of J. Tehranzadeh, MD, University of California at Irvine.
Rheumatoid arthritis. Coronal, T1-weighted magnetic resonance imaging scan shows characteristic pannus and erosive changes in the wrist in a patient with active rheumatoid arthritis. Courtesy of J. Tehranzadeh, MD, University of California at Irvine.
Entrapment neuropathy may result from synovitis about the flexor tendons. Entrapment of the median nerve as it passes through the carpal tunnel leads to decreased sensation on the palmar aspect of the thumb, index finger, and long finger and on the radial aspect of the ring finger; weakness and atrophy of the muscles in the thenar eminence also occurs. Entrapment of the ulnar nerve at the wrist, a less frequent event, causes decreased sensation over the little finger and the ulnar aspect of the ring finger and decreased interosseous muscle strength and mass.
Elbow
Elbow involvement is often detected by palpable synovial proliferation at the radiohumeral joint and is commonly accompanied by a flexion deformity, such as in contractures. Involvement of the olecranon bursa is common, as are rheumatoid nodules in the bursa and along the extensor surface of the ulna (see the image below).
Shoulders
RA commonly involves the shoulders and is manifested by tenderness, nocturnal pain, and limited motion. Initially, swelling occurs anteriorly, but it may be difficult to detect and is present on examination in only a minority of patients at any point in time.
Rotator cuff degeneration secondary to synovitis may limit abduction and rotation. Superolateral migration of the humerus occurs with complete tears. Glenohumeral damage results in pain with motion and at rest and typically leads to severely restricted motion or “frozen shoulder syndrome.” Acromioclavicular arthritis is not as frequent or as disabling as the other manifestations of this disease.
Examination of lower extremities
Ankles and feet
The ankle joint itself is rarely involved without midfoot or MTP involvement. Because it is a mortise joint, it does not often deform. Major structural changes occur in the midfoot and foot as a result of the combination of chronic synovitis and weight bearing. Posterior tibialis tendon involvement or rupture may lead to subtalar subluxation, which results in eversion and migration of the talus laterally. Midfoot disease leads to loss of normal arch contour with flattening of the feet.
The MTP joints are inflamed in most patients and, because of the heavy loads they bear, often become deformed over time. The great toe typically develops hallux valgus (a bunion); subluxation of the phalanx at the MTP joint of the other toes predominantly occurs dorsally. Toes may exhibit compensatory flexion due to a fixed length of the flexor tendons—so-called hammer toes. The second and third metatarsal heads commonly protrude and may become the primary weight-bearing surface at the MTP joints. Calluses and pain upon weight bearing result.
Knees
Affected knees may develop large effusions and abundant accumulation of synovium. Knee effusions and synovial thickening are common in RA and are easily detected during the early course of the disease. Persistent effusions may lead to inhibition of quadriceps function by spinal reflexes, resulting in subsequent atrophy.
Instability may develop after progressive loss of cartilage and weakening of ligaments; deformity may include genu valgus or varus, as well as flexion deformities. The patient’s energy expenditure for standing or walking increases substantially if there are flexion deformities of the knees.
Hips
The hips are commonly involved in RA; however, because of their deep location, their involvement is not always readily apparent early in the course of the disease. Hips are difficult to examine by means of direct inspection or palpation.
Limited motion or pain on motion and weight bearing are the hallmarks of hip involvement. The Patrick maneuver (flexion, external rotation, and abduction) is abnormal in this situation. A flexion deformity may be demonstrable by conducting a Thomas test, which is performed by flexing one hip (with the patient supine) while restricting pelvic motion by keeping the other hip in the neutral position on the examination table. If the hip cannot be maintained in the neutral position, a contracture is present.
Cervical spine
Cervical spine involvement (see the following image) usually affects C1-C2 and has the potential to cause serious neurologic consequences. Patients who are to undergo intubation or procedures that may involve manipulation of the neck should undergo careful evaluation of the cervical spine.
 Juvenile rheumatoid arthritis. Ankylosis in the cervical spine at several levels due to long-standing juvenile rheumatoid arthritis (also known as juvenile idiopathic arthritis).
Juvenile rheumatoid arthritis. Ankylosis in the cervical spine at several levels due to long-standing juvenile rheumatoid arthritis (also known as juvenile idiopathic arthritis).
Neck pain on motion and occipital headache are common manifestations of cervical spine involvement. Most patients with cervical spine involvement (see the image below) have had the disease for more than 10 years.
 Rheumatoid arthritis. Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
Rheumatoid arthritis. Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
Clinical manifestations of early cervical spine disease consist primarily of neck stiffness that is perceived throughout the entire arc of motion. The atlantoaxial joint is a synovial-lined joint and is susceptible to the same proliferative synovitis and subsequent instability seen in the peripheral joints. Patients with severe destruction in the hands (arthritis mutilans) are very likely to have symptomatic cervical spine abnormalities, as are those patients taking significant amounts of corticosteroids for control of RA.
Neurologic involvement in the cervical spine ranges from radicular pain to a variety of spinal cord lesions that may result in weakness (including quadriparesis), sphincter dysfunction, sensory deficits, and pathologic reflexes.
Transient ischemic attacks (TIAs) and cerebellar signs may reflect vertebral artery impingement from cervical subluxation or basilar artery impingement from upward migration of the dens. Tenosynovitis of the transverse ligament of C1 may lead to C1-C2 instability. Myelopathy secondary to rupture of the transverse ligament may lead to neurologic deficits. Radiculopathy is most common at the C2 root, though symptomatic subluxations may occur at any level.
Symptoms of cervical myelopathy are gradual in onset and are often unrelated to either the development or the accentuation of neck pain. When neck pain does occur, it frequently radiates over the occipital region in the distribution of the C1-3 nerve roots. The Lhermitte sign, in which tingling paresthesia that descends through the thoracolumbar spine occurs as the cervical spine is flexed, is typically observed.
For more information, see Rheumatoid Arthritis of the Cervical Spine.
Stiffness, Tenderness, and Pain on Motion
On physical examination, stiffness in patients with RA is determined by limitation of motion, which may vary with the time of day. However, stiffness that is due to articular surface derangement or soft tissue contractures about the joint does not vary with the time of day.
Severe stiffness in the hands may improve with heat, but it is most effectively relieved with active exercise. These modalities reduce stiffness immediately after application, but unfortunately, they do not prevent the return of stiffness.
Direct palpation can elicit joint tenderness, which can vary significantly among patients and with the method of application of force used. To minimize variation over time, the examiner should try to apply approximately the same pressure for each patient examined.
The enlarged synovial membrane, periarticular ligaments, and supporting structures are the major pain-sensitive structures. Muscles may also become tender, but rarely is this due to myositis. Muscle tenderness is not specific for RA. Severe muscle tenderness should suggest another differential diagnosis, including fibromyalgia or a regional pain disorder (see DDx). Bony prominences are generally tender; periarticular structures tend to be more vulnerable to palpation at these sites.
Pain on motion is often used as a surrogate for tenderness in joints that are not readily amenable to direct palpation because of overlying muscle and other tissues. Such areas include the cervical spine, shoulder, and hip.
Pain on motion of the joint may be due to noninflammatory processes that also interfere with the joint’s normal, almost frictionless motion, including damage of cartilage and bone. Additionally, joint instability or subluxation causes pain on motion because of musculotendinous imbalances across the joint. Documenting the positions of motion at which pain occurs can be useful.
Swelling, Deformity, and Limitation of Motion
In RA, enlargement of the synovial membrane is noted on physical examination as thickening of the synovium that may obscure joint margins. This thickening is most evident in the small joints of the hands and feet. In the MCP and MTP joints, the outline of the base of the proximal phalanx may become indistinct, and in the PIP joints of the fingers, a fusiform swelling is noted that is due to the anatomy of the synovial reflections (see the image below).
 Rheumatoid arthritis. Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
Rheumatoid arthritis. Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
If synovial proliferation is abundant, the resultant soft-tissue mass may have a doughy texture on palpation. Such synovial proliferation is commonly identified in the PIP, MCP, elbow, ankle, MTP, and knee joints, as well as in the flexor tendons of the fingers, the common extensor compartment of the dorsal wrist, and the extensor carpi ulnaris tendon sheath.
Joint effusions may also contribute to swelling by distending the joint. When the effusion is put under increased pressure with joint flexion, the synovium may be forced between articular structures, with the result that a portion becomes trapped and separated from the rest of the joint, forming a Baker cyst (see the image below). More fluid is forced into the structure with subsequent loading of the distended joint, and a 1-way valve effect may prevent the fluid from returning to the joint.
 Rheumatoid arthritis. Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
Rheumatoid arthritis. Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
Baker cysts may be seen in most peripheral joints and are most commonly recognized in the knee. [44] The larger the effusion, the more likely it is that a painful cyst will develop in the popliteal fossa. Rupture of a Baker cyst at the knee may resemble acute thrombophlebitis, with distal dissection of inflammatory joint contents along fascial planes as far as the ankle and dorsal foot.
Deformity of the joint may develop over time as articular and supporting structures are damaged by the inflammatory process. By the time deformity has developed, the diagnosis of RA is in little doubt; however, optimal management of RA requires that the inflammatory aspects of the arthritis be recognized before the development of deformity.
Loss of cartilage from proteolytic and mechanical degradation, combined with stretching and weakening of the periarticular ligaments and their attachments, allows forces acting across the joints to deform them. The small joints in the hands and feet are most commonly deformed in this manner; more than 10% of patients with RA develop deformity of the small joints of the hands within the first 2 years of the disease, and at least 33% develop such deformities over time. Joint instability is seen if disruption of supporting structures has occurred.
Limitation of motion occurs as a result of articular surface damage, joint and tendon sheath swelling, or alteration of joint supporting structures. Effusion may limit joint motion through pain or by causing sufficient tightness of the joint capsule to impede joint mobility. Fibrosis involving tendons and muscles may limit normal joint motion and result in flexion contractures. Joint deformities and subluxations invariably limit motion because of mechanical factors.
Extra-articular Manifestations
RA is a systemic disease, and most individuals with this condition experience extra-articular manifestations such as generalized malaise and fatigue. Rarely, a patient presents with extra-articular manifestations before the onset of arthritis. Some of these manifestations are more common in men (eg, pleural involvement, vasculitis, and pericarditis), but overall, the sex distribution of extra-articular manifestations of the disease is similar to that of RA.
Rheumatoid nodules
Rheumatoid nodules occur in approximately 25% of patients with RA, but in fewer than 10% of patients during the first year of the disease. These lesions are most commonly found on extensor surfaces or sites of frequent mechanical irritation.
The olecranon process, the proximal ulna, the back of the heel, the occiput, and the ischial tuberosities are common periosteal sites for rheumatoid nodule development. Nodules may also form in subcutaneous tissues of the fingers, in toe and heel pads, in tendons, and in viscera. Rheumatoid factor (RF) is almost invariably present in patients with rheumatoid nodules; the absence of RF suggests other diagnoses.
Frequently, there is a discrepancy between the level of articular inflammation and the progression of nodule formation. Patients with rheumatoid nodulosis have a great number of nodules, usually subcutaneous, and may have little active synovitis. In a similar fashion, patients whose articular inflammation responds well to treatment with methotrexate may have a seemingly paradoxical rapid increase in the number of nodules.
Effects on organ systems
RA affects several organ systems, as follows:
-
Cutaneous
-
Cardiac
-
Pulmonary
-
Renal
-
Gastrointestinal (GI)
-
Vascular
-
Hematologic
-
Neurologic
-
Ocular
Subcutaneous nodules (rheumatoid nodules) develop in many RA patients whose RF value is abnormal, often over pressure points (eg, olecranon). Vasculitic lesions of the skin may manifest as palpable purpura or skin ulceration (eg, leg ulceration). Additionally, palmar erythema and pyoderma gangrenosum may be noted.
Cardiovascular morbidity and mortality are increased in patients with RA. Nontraditional risk factors appear to play an important role. Myocardial infarction, myocardial dysfunction, and asymptomatic pericardial effusions are common; symptomatic pericarditis and constrictive pericarditis are rare. Myocarditis, coronary vasculitis, valvular disease, and conduction defects are occasionally observed.
RA involvement of the lungs may take several forms, including pleural effusions, interstitial fibrosis, nodules, and bronchiolitis obliterans organizing pneumonia. Methotrexate therapy can induce interstitial fibrosis that may be difficult to distinguish from that which naturally occurs in patients with RA.
The kidneys usually are not directly affected by RA. Secondary involvement is common, including that due to medications (eg, nonsteroidal anti-inflammatory drugs [NSAIDs], gold, and cyclosporine), inflammation (eg, amyloidosis), and associated diseases (eg, Sjögren syndrome with renal tubular abnormalities).
GI involvement, like kidney involvement, is often secondary to associated processes such as medication effects, inflammation, and other diseases. The liver may be affected in patients with Felty syndrome (ie, RA, splenomegaly, and neutropenia).
Vasculitic lesions can occur in any organ, but they are most commonly found in the skin. Lesions may present as palpable purpura, skin ulcers, or digital infarcts.
Some patients with active RA have an anemia of chronic disease. Several hematologic parameters parallel disease activity, including normochromic-normocytic anemia, thrombocytosis, and eosinophilia, though the last of these is uncommon. Leukopenia is a finding in patients with Felty syndrome.
Nerve entrapment is common, as with the median nerve in carpal tunnel syndrome. Vasculitic lesions, mononeuritis multiplex, and cervical myelopathy may cause serious neurologic consequences. Peripheral myopathy may be noted as well.
Keratoconjunctivitis sicca is common in individuals with RA, and this condition is often the initial manifestation of secondary Sjögren syndrome. The eye may also have episcleritis, uveitis, and nodular scleritis that may lead to scleromalacia.
Complications
RA itself is not fatal, but complications of the disease may shorten survival by years in some individuals. In general, RA is progressive and cannot be cured, but in some patients, the disease gradually becomes less aggressive, and symptoms may even improve. However, if bone and ligament destruction and any deformities have occurred, the effects are permanent.
Joint disability and pain with daily life are common. Affected joints can become deformed, and the performance of even ordinary tasks may be very difficult or impossible; these factors can severely affect patients’ quality of life. In addition, RA is a systemic disease that can affect other parts of the body in addition to joints. These effects include the following:
-
Anemia
-
Infections – Patients with RA are at greater risk for infections; immunosuppressive drugs further increase that risk
-
GI problems – Patients with RA may experience stomach and intestinal distress; however, lower rates of stomach and colorectal cancers have been reported in RA patients
-
Osteoporosis – This condition is more common than average in postmenopausal women with RA; the hip is particularly affected; the risk of osteoporosis appears to be higher than average in men with RA who are older than 60 years
-
Lung disease – A small study found a high prevalence of pulmonary inflammation and fibrosis in patients with newly diagnosed RA, but this finding may be associated with smoking
-
Heart disease – RA can affect blood vessels and increase the risk of coronary ischemic heart disease
-
Sjögren syndrome – Keratoconjunctivitis sicca is a common complication of RA; oral sicca and salivary gland enlargement are less common
-
Felty syndrome – This condition is characterized by splenomegaly, leukopenia, and recurrent bacterial infections; it may respond to disease-modifying antirheumatic drugs (DMARDs)
-
Lymphoma and other cancers – RA-associated immune system alterations may play a role; aggressive treatments for RA may help prevent such cancers
-
Juvenile rheumatoid arthritis. Ankylosis in the cervical spine at several levels due to long-standing juvenile rheumatoid arthritis (also known as juvenile idiopathic arthritis).
-
Juvenile rheumatoid arthritis. Widespread osteopenia, carpal crowding (due to cartilage loss), and several erosions affecting the carpal bones and metacarpal heads in particular in a child with advanced juvenile rheumatoid arthritis (also known as juvenile idiopathic arthritis).
-
Rheumatoid arthritis. Rheumatoid changes in the hand. Photograph by David Effron MD, FACEP.
-
Rheumatoid arthritis. Rheumatoid nodules at the elbow. Photograph by David Effron MD, FACEP.
-
Rheumatoid arthritis. Soft-tissue swelling and early erosions in the proximal interphalangeal joints in a patient with rheumatoid arthritis of the hands.
-
Rheumatoid arthritis. Subluxation in the metacarpophalangeal joints, with ulnar deviation, in a patient with rheumatoid arthritis of the hands.
-
Rheumatoid arthritis. Coronal, T1-weighted magnetic resonance imaging scan shows characteristic pannus and erosive changes in the wrist in a patient with active rheumatoid arthritis. Courtesy of J. Tehranzadeh, MD, University of California at Irvine.
-
Rheumatoid arthritis. Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
-
Boutonniere deformity.
-
Rheumatoid arthritis. Anteroposterior radiograph of the knee shows uniform joint-space loss in the medial and lateral knee compartments without osteophytosis. A Baker cyst is seen medially (arrowhead).
-
Rheumatoid arthritis. Ultrasonography-guided synovial biopsy of the second metacarpophalangeal joint of the right hand in a patient with rheumatoid arthritis of the hands. The biopsy needle is seen as a straight echogenic line on the left side of the image in an oblique orientation.
-
Plain lateral radiograph of the normal cervical spine taken in extension shows measurement of anterior atlantodental interval (yellow line) and posterior atlantodental interval (red line).
-
Rheumatoid arthritis. Lateral flexion view of the cervical spine shows atlantoaxial subluxation.
-
Rheumatoid arthritis. Lateral view of the cervical spine in a patient with rheumatoid arthritis shows erosion of the odontoid process.
-
Rheumatoid arthritis. T1-weighted sagittal magnetic resonance image of the cervical spine shows basilar invagination with cranial migration of an eroded odontoid peg. There is minimal pannus. The tip of the peg indents the medulla, and there is narrowing of the foramen magnum due to the presence of the peg. Inflammatory fusion of several cervical vertebral bodies is shown.
-
Sagittal T2-weighted magnetic resonance image of cervical spine in same patient as in previous image. Compromised foramen magnum is easily appreciated, and there is increased signal intensity within upper cord; this is consistent with compressive myelomalacia. Further narrowing of canal is seen at multiple levels.
-
Rheumatoid arthritis. Lateral radiograph of the same patient as in Images 4-5. Midcervical vertebral-body fusions are shown. The eroded peg is difficult to visualize, but inferior subluxation of the anterior arch of C1 is shown.
-
Lateral radiograph of a normal cervical spine shows the McGregor line. The odontoid tip should not protrude more than 4.5 mm above the line, which is drawn from the posterior edge of the hard palate to the most caudal point of the occiput.
-
Normal lateral magnified radiograph of the cervical spine shows the Ranawat method of detection of cranial settling. This method is used to measure the distance from the center of the pedicles (sclerotic ring) of C2 to a line drawn connecting the midpoints of the anterior and posterior arches of C1. (Normal values are 15 mm or greater for males and 13 mm or greater for females.)
-
Lateral radiograph of the cervical spine shows how the cervical height index (CHI) is calculated. The distance from the center of the sclerotic ring of C2 to the tip of the spinous process of C2 (dotted line) is measured. This is then divided into the distance from the center of the sclerotic ring of C2 to the midpoint of the inferior border of the body of C7. A CHI of less than 2 mm is a sensitive predictor of neurologic deficit.
-
X-ray shows total hip replacement, with prosthesis, in patient with osteoarthritis.
-
Rheumatoid arthritis. This gross photo shows destruction of the cartilage and erosion of the underlying bone with pannus from a patient with rheumatoid arthritis.
-
Rheumatoid arthritis. The hallmark of rheumatoid arthritis is a perivascular mononuclear cell infiltrate in the synovium (pictured here). The early stages are noted to have plasma cells as well, and syphilis needs to be part of the differential diagnosis.
-
Rheumatoid arthritis. The inflammation involved in rheumatoid arthritis can be intense. It is composed of mononuclear cells and can resemble a pseudosarcoma.
-
Rheumatoid arthritis. A 72-year-old man with long-standing rheumatoid arthritis developed blue-grayish discoloration of his skin. He had been on hydroxychloroquine for approximately 15 years. The diagnosis was hydroxychloroquine-related hyperpigmentation. Image courtesy of Jason Kolfenbach, MD, and Kevin Deane, MD, Division of Rheumatology, University of Colorado Denver School of Medicine.
-
Rheumatoid arthritis. A 64-year-old woman with rheumatoid arthritis has developed nodules on the dorsal and volar aspect of her fingers, as well as the posterior aspect of her heels. The diagnosis is rheumatoid nodules with methotrexate-induced accelerated nodulosis. Image courtesy of Jason Kolfenbach, MD, and Kevin Deane, MD, Division of Rheumatology, University of Colorado Denver School of Medicine.
-
Rheumatoid arthritis. A 64-year-old woman with rheumatoid arthritis has developed nodules on the dorsal and volar aspect of her fingers, as well as the posterior aspect of her heels. The diagnosis is rheumatoid nodules with methotrexate-induced accelerated nodulosis. Image courtesy of Jason Kolfenbach, MD, and Kevin Deane, MD, Division of Rheumatology, University of Colorado Denver School of Medicine.